Oral Presentation 51st International Society for the Study of the Lumbar Spine Annual Meeting 2025
AI-Driven Phenotyping to Investigate Biopsychosocial Factors Affecting Return-to-Work in Chronic Low Back Pain Workers (#MP-7b)
INTRODUCTION
Chronic low back pain (cLBP) is a prevalent musculoskeletal disorder and the leading cause of disability worldwide1, with work-related cases representing a significant challenge for occupational health2. Although artificial intelligence (AI) has been applied to phenotypic profiling based on behavioural, psychological, and social factors3,4, the link between these biopsychosocial phenotypes and work-related outcomes in cLBP remains largely unexplored5. This study aims to investigate the biopsychosocial factors impacting work functioning in individuals with cLBP through AI-driven patient phenotyping. We hypothesize that distinct subgroups will emerge, each defined by specific levels of disability and biopsychosocial factors related to work limitations.
METHODS
Baseline data for workers affected by cLBP were collected through a comprehensive assessment of demographic, clinical, and occupational factors. Patient-reported outcome measures (PROMs) included the Oswestry Disability Index (ODI), Visual Analog Scale (VAS), Work Ability Index (WAI), WHO Well-Being Index (WHO-WBI), Pittsburgh Sleep Quality Index (PSQI), Nordic Score, and Patient Health Questionnaire-2 (PHQ-2). Phenotypic clusters were identified using hierarchical agglomerative clustering with Ward’s linkage and Euclidean distance. Statistical tests evaluated differences in work-related outcomes, absenteeism, pain, and psychological distress between clusters, focusing on significant variations in continuous and categorical data distributions.
RESULTS
A total of 304 patients were included. Two distinct clusters of patients were identified, accounting for 51% (n=155) and 49% (n=149) of the total sample, respectively (Fig.1 and Fig.2). Patients in Cluster 2 exhibited significantly higher absenteeism compared to Cluster 1 (17 vs. 5.22 days, p<0.05), lower WAI (33.34±6.84 vs. 38.96±4.31, p<0.05), worse pain-related outcomes in terms of higher VAS (5.98±2.06 vs. 4.48±2.48, p<0.05) and ODI (33.52±16.56 vs. 20.08±13.59, p<0.05) (Fig.3), more frequent occupational exposure to manual handling of loads (84% vs. 16%) and higher psychological distress assessed through PHQ-2 (70% vs. 30%). In contrast, Cluster 1 showed lower absenteeism, better work ability, less pain, lower exposure to manual handling of loads, and reduced psychological distress compared to Cluster 2.
DISCUSSION
As a major cause of disability and productivity loss, work-related cLBP presents a multifaceted challenge in occupational health, emphasizing the need to understand individual variations in occupational outcomes. Cluster analysis effectively differentiated two clusters of workers with cLBP, with Cluster 2 exhibiting worse absenteeism and pain-related outcomes. These findings highlight the potential of AI-driven approaches to guide personalized interventions tailored to specific biopsychosocial profiles, aiming to enhance clinical outcomes and work capacity among workers with cLBP. Future studies should investigate the long-term impact of phenotype-specific interventions on workforce retention and productivity in this population.
Fig. 1. Hierarchical clustering dendrogram of biopsychosocial profiles in cLBP patients.

Fig. 2. Spatial distribution of chronic low back pain patient clusters visualized using the Uniform Manifold Approximation and Projection method.
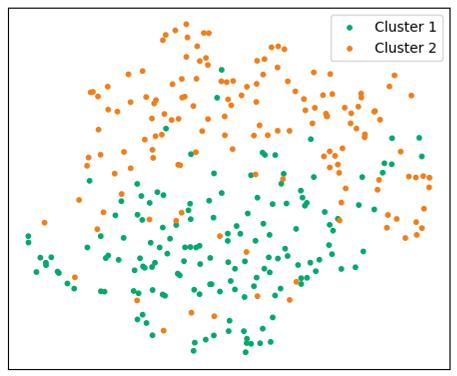
Fig. 3. Mean values of key numerical features relevant for phenotyping (p<0.05). The left panel displays absenteeism data, showing the number of workdays missed due to cLBP across different time frames for Cluster 1 and Cluster 2. The right panel presents mean scores for VAS, ODI, and WAI in both clusters, highlighting significantly worse outcomes in Cluster 2 for each measure.

- Wu et al., Ann Transl Med; 2020.
- Jegnie et al., J Environ Public Health; 2021
- Rabey et al., Clin J Pain; 2016
- Garcia et al., Health Soc Care Community; 2022
- Carlesso et al., Can J Pain; 2021