Poster Presentation 51st International Society for the Study of the Lumbar Spine Annual Meeting 2025
Can screw loosening be predicted by measuring the insertion torque even in non-osteoporotic bone? An in vitro study (#224)
Introduction
Pedicle screw loosening is a major complication, with up to 60% in osteoporotic and 1-15% in non-osteoporotic patients [1,2]. Even in young patients, it sometimes remains unclear if screw augmentation should be performed and if surgically applied distraction forces need to be limited. Thus, it would be beneficial for the surgeon to assess the risk of screw loosening intraoperatively, but without X-ray exposure if possible. Whereas in vitro the risk of screw loosening can be estimated by pullout or with more physiological bending tests [3], this is not possible in vivo. To find a prediction tool, the purpose of this in vitro experiment was to correlate the screw insertion torque with a bending force necessary to create screw loosening in non-osteoporotic vertebrae.
Methods
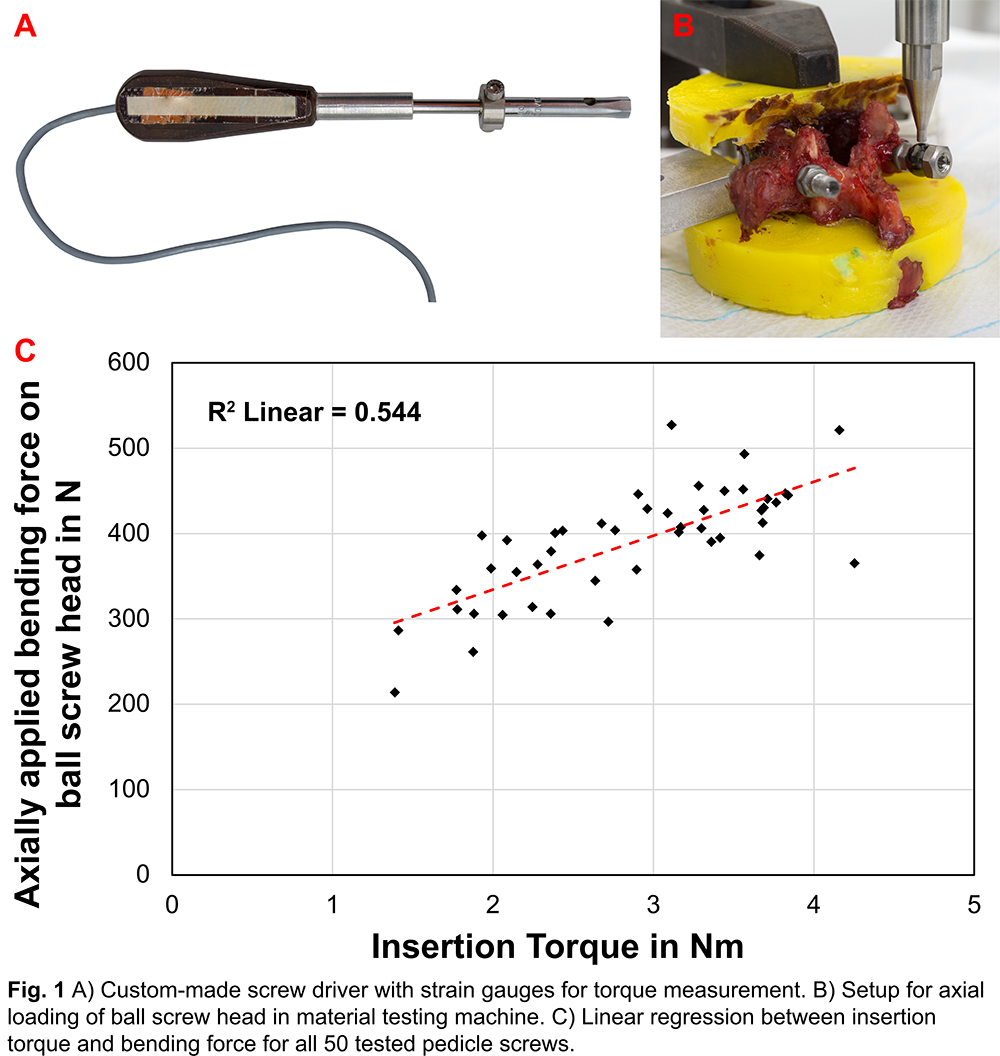
In total, 50 pedicle screws were implanted into both left and right pedicles of 25 single vertebrae (11 donors, mean age 40±9, L1-L4) with a median bone mineral density (BMD) of 142 (120-186) mgCaHA/cm3 assessed by QCT. After pre-drilling (2.5x20), the largest possible screw (5.5x40, 5.5x45, 6.5x40, 6.5x45, or 6.5x50) was implanted into the pedicle while measuring the insertion torque (Fig1A). Both endplates were embedded in PMMA and fixed in a material testing machine. A bending force was applied on the screw head until reaching a displacement of 1 mm (5 N pre-load; 10 mm/min; Fig1B). Afterwards, first a univariate and then a multiple mixed linear model were calculated (SPSS; significant level p < 0.05).
Results
The bending force increased linearly with the insertion torque (multiple; p = 0.0002; Fig1C). The length and the diameter of the screw as well as the vertebral level had a significant impact on the bending force in the univariate model (p < 0.0001) but not in the multiple one. BMD did not affect the bending force (univariate; p = 0.2483). The screw diameter showed a slight trend for the multiple model (p = 0.0584).
Discussion
For osteoporotic bone, the data are controversial but for non-osteoporotic bone the insertion torque seems to function sufficiently as a predictor of screw loosening. The results suggest that the linear correlation of insertion torque and bending force can be used to calculate the maximum allowable distraction and, as an alternative method, to estimate the risk of screw loosening in vivo. Additional information (e.g., need for augmentation) could be provided to the surgeon as well as surgical outcomes and patients’ safety improved. This is potentially a simple, intra-operative, and radiation free method. The static test method used is a limitation but was intended to simulate inter-operative distraction. In further experiments, the procedure should be further optimized for clinical use with additional screw types.
- Galbusera F, Volkheimer D, Reitmaier S, Berger-Roscher N, Kienle A, Wilke HJ. Pedicle screw loosening: a clinically relevant complication? Eur Spine J. 2015;24(5):1005-16.
- El Saman A, Meier S, Sander A, Kelm A, Marzi I, Laurer H. Reduced loosening rate and loss of correction following posterior stabilization with or without PMMA augmentation of pedicle screws in vertebral fractures in the elderly. Eur J Trauma Emerg Surg. 2013;39(5):455-60.
- Bostelmann R, Keiler A, Steiger HJ, Scholz A, Cornelius JF, Schmoelz W. Effect of augmentation techniques on the failure of pedicle screws under cranio-caudal cyclic loading. Eur Spine J. 2017;26(1):181-8.